What Is Osteoarthritis?
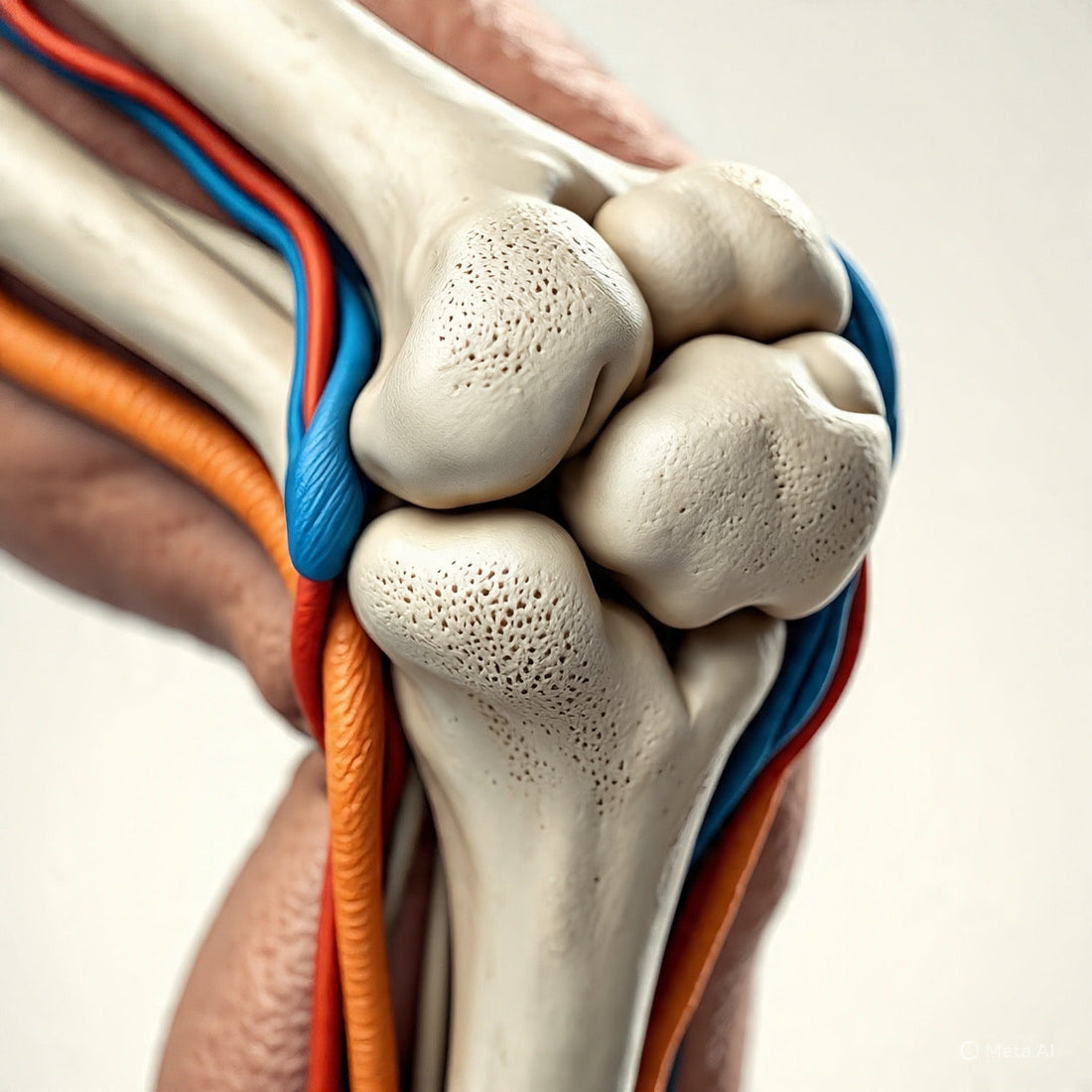
Osteoarthritis (commonly called **OA**) is the most common form of arthritis. It occurs when parts of a joint gradually wear down over time.
In a healthy joint, cartilage (a smooth cushion) covers the ends of bones and allows them to glide smoothly. When cartilage is damaged, bones may rub together, leading to pain and stiffness. Over time, the soft tissues (ligaments, joint lining) and the bone beneath the cartilage may also be affected.
Why Does It Happen?
Several factors can increase the chance of developing OA, or make it worsen:
- Getting older — repair mechanisms slow down, and wear accumulates.
- Being overweight — adds extra load to joints, especially knees and hips.
- Past joint injury or surgery — damaged joints are more vulnerable.
- Repeated or heavy use of a joint — e.g. occupational strain, sports overuse.
- Joint alignment or shape issues — uneven pressure inside the joint.
- Weak muscles around the joint — muscles help stabilize and relieve stress on the joint.
What Do People With OA Feel?
What You Might Notice (Symptoms)
- Joint pain — often worse after movement or activity; sometimes worse at night.
- Stiffness — especially after resting or staying still; usually brief (often < 30 minutes).
- Swelling or puffiness around the joint after activity.
- Grinding, crackling, or “creaky” sensation when moving the joint.
- Reduced range of motion — difficulty bending or straightening, trouble in daily tasks.
What a Doctor May See
- Tenderness around the joint.
- Joint swelling or visible puffiness.
- Less motion in the joint compared to normal.
- Bone changes or small bony bumps (spurs / osteophytes) on imaging or by touch.
What Can You Do? How to Manage Osteoarthritis
Although there is currently **no cure** for OA, many steps can help reduce pain, slow progression, and keep you mobile.
- Learn about the condition — understanding OA helps you and your care team make good choices.
- Stay active in gentle ways — walking, swimming, cycling, and regular movement help maintain joint function. (Start gradually.)
- Strengthen muscles around the joint — strong muscles support the joint and reduce strain; ask a physical therapist for guidance.
- Maintain a healthy weight — losing even a small amount can ease the load on your joints.
- Use supports if needed — braces, special shoes, walking sticks, or canes can help relieve stress on the joint.
- Use heat or cold — warm packs may relieve stiffness; cold packs can reduce swelling.
- Modify activities — avoid or reduce tasks that overly strain the joint; take breaks; adapt how you do things.
- Get professional help — physical therapists, occupational therapists, doctors can help refine your plan and monitor progress.
- Consider procedural or surgical options when necessary — in moderate to severe cases, doctors may suggest injections, realignment surgery, or joint replacement.
References & Credit Sources
“Osteoarthritis Symptoms, Causes & Risk Factors” — NIAMS. :contentReference[oaicite:0]{index=0}
“Osteoarthritis: Diagnosis, Treatment, and Steps to Take” — NIAMS. :contentReference[oaicite:1]{index=1}
“Nonpharmacologic – Osteoarthritis Action Alliance” — OA Action. :contentReference[oaicite:2]{index=2}
“Osteoarthritis Treatment Guidelines from Six Professional Societies” — PMC NCBI. :contentReference[oaicite:3]{index=3}
“Non-pharmacological and non-surgical interventions to manage OA” — PMC NCBI umbrella review. :contentReference[oaicite:4]{index=4}
“EULAR recommendations for the non-pharmacological core management of hip and knee OA” — PMC. :contentReference[oaicite:5]{index=5}
“Non-surgical management of hip and knee osteoarthritis” — PMC NCBI. :contentReference[oaicite:6]{index=6}
“What Is Osteoarthritis? — Mayo Clinic” — Mayo Clinic overview. :contentReference[oaicite:7]{index=7}